Discovery is first to target the bacterial "persisters" responsible for many lingering illnesses
Researchers from the Wyss Institute for Biologically Inspired Engineering at Harvard University and from Boston University have developed an effective, low-cost approach to treating chronic bacterial infections, such as staph and urinary tract, and potentially even strep and tuberculosis. Their findings appear in the May 12 issue of Nature.
Chronic and recurrent infections are typically caused by bacterial “persisters” — a small subpopulation of bacteria that manage to survive an antibiotic onslaught by essentially shutting down and “sleeping” through it, even as their counterparts, who are awake, are killed off.
As a result, the patient initially appears to be fully recovered, but over the course of weeks, or even months, the persisters start returning to life, often stronger and more aggressive than ever before, and the illness is back. Bacterial persistence is a major obstacle to the successful treatment of infectious diseases. It can stretch illnesses out over months, cause infections to spread to kidneys and other organs, and send treatment costs soaring. Given its significant negative impact, bacterial persistence has become a growing area of research, yet to date, no treatment that directly targets persisters has been developed.
Unlike antibiotic resistant bacteria, whose ability to withstand drug treatments is based on genetic differences, persisters are genetically identical to the other members of their bacterial community. What separates them from the pack is their ability to switch into power-save mode.
But a research team led by James J. Collins, Ph.D., has now discovered an inexpensive and effective way to rouse these bacterial sleepers, using sugar to stimulate them into an active state in which they are just as vulnerable to antibiotics as the others in their community.
Collins is a core faculty member of the Wyss Institute, a professor of Biomedical Engineering at Boston University, and a Howard Hughes Medical Institute investigator. Kyle Allison, of the Howard Hughes Medical Institute and Boston University, was the first author, with Mark Brynildsen, an Assistant Professor in the Department of Chemical and Biological Engineering at Princeton University, a contributing author.
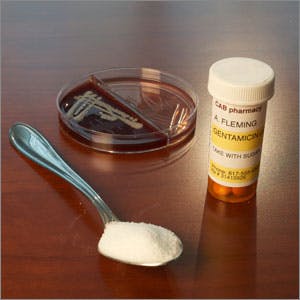
Their approach consists of adding sugar to the antibiotic. The sugar acts as a stimulant, essentially turning the bacteria’s normal responses, such as dying when confronted by a killer antibiotic, back on. Allison likens the effect of the sugar to a bacterial cup of coffee or the shriek of an alarm clock.
Using this strategy on E. coli bacteria, which can cause urinary tract infections, the team was able to eliminate 99.9 percent of the persisters within just two hours, as opposed to no elimination without sugar. The approach was similarly effective in killing the bacteria that causes staph infections. “Our goal was to improve the effectiveness of existing antibiotics, rather than invent new ones, which can be a long and costly process,” says Allison.
These findings have the potential to improve the lives of untold numbers of people who struggle with nagging infections, while also reducing healthcare costs substantially. But, the most significant impact could ultimately be felt people around the world who suffer from tuberculosis, which is the next focus of Allison and Collins’s research.
TB, which is a chronic bacterial infection that affects the lungs, causes more deaths than any other infectious disease. The World Health Organization reports that approximately 4,700 people die from TB every day. Treatment typically takes five to nine months.