Dyno Therapeutics is developing optimized AAVs to enable a new generation of more effective, safer gene therapies across a large spectrum of diseases.
The Problem
Gene therapies, in contrast to drug-based therapies, use actual genes to treat, prevent, or cure diseases. In many cases, this means that a healthy copy of a gene that has become dysfunctional in a patient’s genome is reintroduced into their body. To deliver therapeutic genes to the target tissues that are most affected by a disease, the protein shell (capsid) of Adeno-associated viruses (AAV) has become a go-to vehicle. AAVs are non-disease-causing and, through past engineering efforts, have been modified so that they do not integrate into the genome of target cells with potentially damaging consequences, but reside outside the genome where the delivered DNA directs expression of the therapeutic gene.
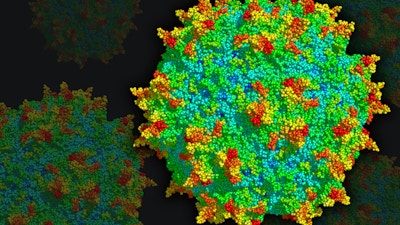
Different subtypes of AAV capsids can deliver DNA to a spectrum of cell and tissue types that varies between capsids. This is due to the organization of the icosahedron-shaped capsid that forms an envelope around the DNA payload, and that via protruding spike structures interacts with specific molecules on target cells. A major challenge in many gene therapies is entry of AAVs into cells that are not supposed to be targeted. This can reduce the amount of the therapy that is successfully delivered to disease-affected tissues, and cause undesired responses in other cell and tissue types. Importantly, among off-target cells are also immune cells, which then can trigger both a dangerous immune response, as well as an immune memory that can prevent the gene therapy from being provided a second time, should it be necessary.
Our Solution

To overcome these limitations, a Wyss Institute team led by former Staff Scientist Eric Kelsic and Core Faculty member George Church took a systematic, unbiased synthetic biology approach to create AAV capsids with different or more selective cell type and tissue-targeting abilities. In what became the team’s core technology built around machine learning and current DNA synthesis methods, they performed a so-called “Wide Search” to generate multiple variants of the gene encoding the AAV capsid-forming protein in which all of its amino acid building blocks were individually mutated. Infection of these AAV variants into human cell lines in vitro and mice in vivo led to the identification of amino acids that could be variably tuned without compromising capsid stability, while shifting target cell and tissue specificities.
Leveraging data from this Wide Search, the team collaborated with Google Research to develop a massively parallel, AI-driven rapid evolution approach they called “Deep Search,” which identified specific combinations of changes that further increased target cell specificity and enhanced the immune evasion potential of synthetic AAV variants. Using a classic synthetic biology paradigm, the researchers performed multiple iterations of the “design-build-test cycle” to inform the design of AAV variants in an upcoming cycle with findings obtained in the previous cycle. In a vast effort, the researchers generated, tested, and analyzed about 200,000 virus variants, and thus created cutting-edge methodology and an invaluable resource for the development of future delivery vehicles for gene therapies.
Product Journey
With the ambitious goal of solving in vivo gene delivery challenges for patients, Kelsic, the team’s computational expert Sam Sinai, and Church spun their novel AAV platform technology out of the Wyss Institute and Harvard University by founding Dyno Therapeutics in 2018. The company, with Kelsic as its CEO and Sinai its Head of Computation, remained in stealth until its official launch in 2020, but before that established partnerships with leading gene therapy developers, including Novartis, Sarepta Therapeutics, Roche and Spark Therapeutics, as well as Astellas Pharma. These partnerships provided Dyno with $58 million in upfront and early-milestone payments, and could potentially result in several billion dollars in future milestone and royalty payments. In addition, Dyno raised $9 million in seed funding before its official launch and, following that, $100 million in series A funding.
In 2023, at the annual meeting of the American Society of Gene & Cell Therapy, Dyno announced “Dyno bCap1TM,” a breakthrough AAV gene delivery vector capable of targeting up to 20% of neurons throughout the brain in non-human primate models when administered at low doses. Dyno bCap1TM dramatically increases the delivery of DNA payloads to the central nervous system upon crossing the blood-brain barrier, and reduces targeting of the liver (a common AAV target tissue) compared to leading natural AAV capsids. At the same conference, Dyno also announced critical improvements to its machine-learning algorithms for the sequence design of AAV capsids, and optimized AAV capsids for best-in-class delivery of ocular gene therapies.
Impact
After its highly successful start in the startup world, Dyno is focused on becoming a leading gene therapy delivery partner, and enabling other companies across the ecosystem to bring gene therapies to patients. Moving full steam ahead in its endeavors, Dyno has built a scientific workforce of more than 110 full-time employees at its self-designed and custom-built headquarters in Watertown, Mass., and was included in the 2022 and 2023 Forbes List of America’s Best Startup Employers.
In addition, in 2020, Dyno was named a “2020 Startup of the Year” by Xconomy. In 2021, Endpoints News named Dyno one of the “2021 Endpoints 11” most promising biotech startup companies, and the New England Venture Capital Association named Dyno an “Emerging Life Science Company of the Year.” Also in 2021, Eric Kelsic was included in the “20 under 40” list by Endpoints News, which recognizes the next generation of biotech leaders.
Dyno is pursuing additional partnership opportunities with genomic medicine companies to enable a new generation of more effective, safer gene therapies by harnessing its optimized AAV capsids.