By Eriona Hysolli
Gene therapy has been recently reinvigorated through advances in genome editing techniques that allow fast and efficient gene correction and replacement in addition to gene introduction into cells in a culture dish. However, in vivo delivery of genes and gene editing tools remains challenging and presents a major hurdle in current treatment efforts – one that is the principal research focus of a Wyss team led by George Church, PhD, a founding Core Faculty of the Institute and Professor at Harvard Medical School and MIT.
Current delivery methods are broadly categorized in viral vs. non-viral systems. The viral category includes retrovirus, lentivirus, adenovirus, Epstein–Barr, herpes simplex and pox viruses among others, whereas non-viral protocols (both physical and chemical) include electroporation, DNA bombardment, ultrasound, magnetofection and hydrodynamic, or cationic and lipid polymers. Generally non-viral methods suffer from highly inefficient targeting while viral-based methods offer advantages related to delivering larger cargo in a relatively efficient fashion, but can be highly immunogenic and unsafe.

Enter AAV.
AAV, or adeno-associated virus, is currently the main viral vector that researchers use and further develop for gene therapy because it is considered to be non-pathogenic to humans and because it has been successfully altered to prevent its integration into the genome, thus eliminating DNA damage and unpredictable consequences. First discovered in 1965 in collected cultures from rhesus monkey kidney cells, AAV contains a single-stranded DNA genome in which therapeutic cargo sequences within certain size limits can be fitted within the flanking inverted terminal repeats, DNA elements containing a sequence of nucleotides followed by its reverse complement used by the virus to demarcate its genome and could enhance DNA exchange with other DNA sequences through recombination, or circularize the genome itself. The AAV genome consists of the rep and cap genes responsible for the viral life cycle and the formation of the capsid shell surrounding the genome, respectively. The capsid proteins assemble in an icosahedron shape with spikes sticking out of the structure to mediate interaction with proteins present on the surface of cells that the virus is targeting. These spikes are also responsible for giving different AAV types their specificity towards different cells.
AAV has moved into the focus of several companies that are developing treatments of different diseases, including blindness in the form of the rare Leber Congenital Amaurosis and Hemophilia B, a hereditary bleeding disorder. Highlighting the potential of AAV, Glybera, a proven but costly and recently discontinued treatment in Europe, had become the first approved gene therapy by enabling AAV1-mediated delivery of functional LPL copies in patients with mutations in this gene causing the rare metabolic disease lipoprotein lipase deficiency (LPLD).
Despite the versatility, relative safety and popularity of AAV, several challenges remain that still impede its mainstream use in the clinic. At the Wyss Institute, researchers are engineering novel AAV vectors with “designer” functions, and also leveraging new synthetic biology approaches to directed evolution and mutagenesis to further engineer AAV serotypes, or variants, into efficient, highly specific and non-immunogenic delivery vehicles.
AAV and Immune Response
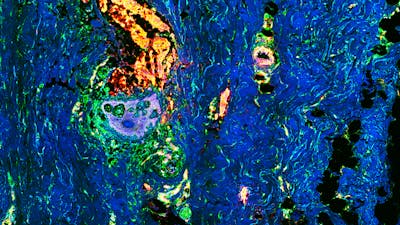
First, administering a large dose of the virus poses a health risk with inflammation and liver toxicity observed in participants of ongoing clinical trials, such as recent Hemophilia B trials. “The aim is to engineer the virus in a simple way to suppress inflammation and prevent another Gelsinger case,” said Ying Kai Chan, Ph.D., a Postdoctoral Fellow in Church’s team referring to the 1999 case of Jesse Gelsinger, who died from the strong inflammatory and immune response triggered by adenovirus-based gene therapy, one of the earliest gene therapy vectors used. While AAV is the safest tested virus vector, it is still subject to immune surveillance and can set off a rapid inflammatory and immune response. This has led to an abnormal increase of well-known indicators of liver damage, in patients of several AAV clinical trials. In one project at the Wyss Institute, Chan is using animal models to test engineered AAVs that evade the immune system. Chan has observed promising results indicating reduced inflammation and toxicity in liver and eye tissues of mice after using the engineered AAV vectors. This may pave the way for a generation of safer and more efficacious AAV vectors for gene therapy and mitigate the fear of deleterious inflammatory effects when undergoing gene therapy.
AAV Diversity
Another problem that Wyss researchers are trying to find solutions for is that of cell- and tissue-type specificity. There are an estimated 12 natural AAV serotypes or variants that can infect human cells, each expressing a separate antigen on its surface that is recognized by the immune system, which then deploys different antibodies to neutralize them. Each of the serotypes can infect human tissues, but their infection efficiencies often remain low. Thus a generally expanded repertoire of more cell and tissue-specific and variants allowing higher infection rates would be desirable to achieve better delivery of therapeutic nucleic acid sequences. This becomes paramount if only one cell type within a complex tissue made of many different cell types is to be specifically targeted for treatment. A larger repertoire of AAV variants will also be helpful to tackle perhaps the greatest challenge in the AAV field: if an individual is exposed to any variant of the virus, the accompanying immune response will create a memory of that infection and render the individual resistant to subsequent ones. This hurdle is addressed by screening participants for the presence of AAV antibodies, and either excluding resistant ones – a large fraction of the population needing gene therapy – or administering powerful but often toxic immunosuppressants.
In order to generate more efficient, highly specific and less immunogenic AAV variants, the Wyss Institute’s AAV team is leading the way in developing strategies able to design new and more tailored virus variants. Efforts by other groups to engineer AAV involve structure based design, random mutagenesis and more recently reconstructing the ancestral sequence of the capsid gene by analyzing all known AAV serotypes and deriving the oldest sequence that gave rise to the present variants. This sequence is thought to be less immunogenic than current AAV serotypes as the human population has not recently been exposed to this archaic AAV. Church however prefers a forward looking evolutionary and non-biased approach which may provide a larger reservoir of AAVs with unique abilities.
Eric Kelsic, Ph.D., a Wyss Staff Scientist on Church’s team together with Pierce Ogden, a Graduate Student in Harvard’s Biological and Biomedical Sciences program have worked out a scheme that is able to evolve new and improved AAV variants very effectively. “Essentially we are taking a data driven approach to protein engineering by leveraging the modern technologies of DNA synthesis and sequencing to generate mutations in the AAV genome that improve performance over natural viruses” explains Kelsic. In principle their strategy involves synthesizing AAV sequences with insertions, substitutions or deletions at positions throughout the AAV capsid and using virus particles containing the synthetic sequences to infect a panel of mouse and human cells. The team will analyze infected cells and recover the sequences of the best performing variants and correlate these novel sequences with unique preference for a particular cell type (tropism), high infectivity rate, and immune system evasion. This massive synthetic biology experiment is repeated with the most favorable AAV candidates in multiple cycles to identify combinations of genetic changes that satisfy all criteria of a desired AAV variant.
Kelsic and Ogden have so far focused on engineering the capsid gene of the AAV2 serotype, which if left unaltered, displays a broad tropism towards different cell types. Using this data-driven approach they have discovered that certain external regions forming the extruding spikes of the capsid protein structure, which are the viral structures known to confer tropism and can be recognized by immune cells, are more tolerant to changes in the DNA sequence than the internal regions making up the central core of the viral capsid, a finding that agrees with known AAV diversity. Kelsic and Ogden are now developing assays that will allow them to measure the effects of capsid mutations for in vivo delivery in mice in order to understand viral preferences for certain cell types and tissues, as well as to enable engineering of desirable properties such as being able to cross the blood brain barrier, a process that cannot be achieved by the majority of AAV serotypes. In future work they plan to apply machine learning, or advanced computing and analysis of data without biased computer programs, to model the effect of changes to the capsid sequence, and to investigate novel variants in human organoid structures and human organs-on-chips to assess differences in infection rate between species. There are reported differences between mouse and human infection efficiencies for some cells and tissues, and further improvement of human-specific infectivity is needed to strengthen AAV-mediated therapeutic findings coming from data analysis of mouse models. The combined efforts of Kelsic, Chan and Ogden pave the way for a generation of safer and more efficacious AAV vectors for gene therapy and could help mitigate the deleterious inflammatory effects during AAV-mediated gene therapy.
AAV Applications
Wyss team member Denitsa Milanova, Ph.D., a Postdoctoral Fellow who works with Church, is already utilizing current and novel AAV vectors in ongoing efforts to deliver factors that reverse skin aging and thus prevent age-related skin disease progression. Milanova is pioneering new gene therapy approaches utilizing ultrasound for non-invasive delivery to improve skin health and appearance. She is collaborating with a number of Harvard-affiliated faculty and hospitals including Carl Schoellhammer, PhD, a Postdoctoral Fellow at the MIT Langer lab and the Mandinova lab at the Massachusetts General in order to develop a novel human skin tissue model that will allow her to screen for genes restoring a healthy and youthful skin. Milanova and Schoellhammer are combining ultrasound technology with AAV to facilitate a needle-less and painless delivery of the virus to skin. “What is special about our strategy is targeting a cocktail of AAVs with ultrasound into different skin cell types in order to make the old cells behave like young”, says Milanova. She is assessing overall skin appearance and biomarker expression to test the rejuvenation effects of this technology.
The Wyss AAV team led by Church is exploring the great potential of AAV as a gene delivery tool and rapidly engineering it into a new and improved vector entity that is able to accommodate the demands and the development pace of safe gene therapy technologies.