Treatments targeting the body’s immune system have become a powerful weapon in our cancer-fighting arsenal. But immunotherapy is just getting started.
By Lindsay Brownell

Prior to the 1990s, the treatment options available to cancer patients were so disfiguring, toxic, or ineffective that many chose to forego therapy altogether. That changed with the approval of the first immunotherapies: Rituxan for lymphoma and Herceptin for breast cancer. These drugs consist of antibodies that bind to molecules on their target cancer cells’ membranes, which activates a patient’s immune system to attack them. This approach has sparked a revolution not only in cancer treatment, but in using immune-targeted strategies to address a variety of inflammatory diseases. Several Wyss Institute labs are working to overcome roadblocks in the field and develop the next generation of immunotherapies through the Institute’s Validation Project program.
T-cell therapy for all tumors
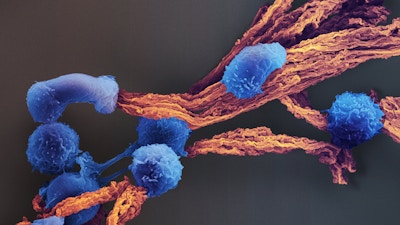
Instead of delivering antibodies, another type of immunotherapy called adoptive T-cell therapies involves extracting T cells from patients, engineering them to target the patient’s particular form of cancer, and delivering them back into the blood to enhance the immune response. These therapies are remarkably effective against blood cancers, but so far have shown limited success against solid tumors. A team in the lab of Core Faculty member Dave Mooney, Ph.D., has developed a technique that allows them to metabolically “tag” the surface of T cells with cytokines, which enhance the anti-tumor activity of immune cells. This technique avoids the negative side effects that prevent cytokines from being delivered systemically, and effectively treated both solid and liquid tumors in mice as an add-on to CAR-T cell therapy. This technology could boost the efficacy of multiple forms of cellular therapies, and is currently being de-risked.
“Waking up” deactivated macrophages

T cells aren’t the only immune cells involved in fighting off invaders – macrophages, or white blood cells, constantly patrol the body for threats, and are often the first cells to flock to a tumor. However, tumors secrete molecules that deactivate macrophages upon arrival, to the point that as much as 50% of a tumor’s mass is made of macrophages.
A Wyss team led by Core Faculty member Samir Mitragotri, Ph.D., is solving this problem by attaching tiny “backpacks” – disc-shaped nanoparticles loaded with proinflammatory cytokines – to macrophages. When infused into the body, these macrophages can switch those inside a tumor from an “off” state to an “on” state, reactivating them against the cancer. The team is now investigating this technology for use in treating glioblastoma, as macrophages are able to penetrate the infamously tough blood-brain barrier that prevents most drugs from reaching the brain.
Deliberately designing vaccines with DNA
Although immunotherapies are a relatively new technology, a much older technique also works by stimulating the body’s immune response: vaccines. Many labs and companies are developing personalized cancer vaccines that preemptively train the immune system to recognize and kill cancer, but so far none are on the market.

These vaccines typically contain an antigen (a protein fragment taken from a patient’s cancer cells that activates antigenpresenting cells [APCs]) and an adjuvant (a molecule that enhances the immunestimulating response of APCs). Both an antigen and an adjuvant are required for an effective tumor-specific response, but little is known about the optimal method of presenting these components to APCs. Core Faculty member William Shih, Ph.D., and his lab have created a solution composed of the stuff of life itself: DNA.
Their DoriVac technology consists of folded sheets of DNA origami whose configuration can be controlled down to the nanoscale. This precision has allowed them to experiment with different arrangements of antigens and adjuvants in cancer vaccines, and they have identified patterns that produced strong tumorinhibiting responses in mice and could be combined with other cancer treatments for better outcomes. The team is de-risking their innovation for commercialization.