New findings show programmable biomaterials can be delivered using needle injection to induce an immune response and fight deadly diseases
Credit: Wyss Institute at Harvard University
(BOSTON/CAMBRIDGE) — One of the reasons cancer is so deadly is that it can evade attack from the body’s immune system, which allows tumors to flourish and spread. Scientists can try to induce the immune system, known as immunotherapy, to go into attack mode to fight cancer and to build long lasting immune resistance to cancer cells. Now, researchers at the Wyss Institute for Biologically Inspired Engineering at Harvard University and Harvard’s School of Engineering and Applied Sciences (SEAS) show a non-surgical injection of programmable biomaterial that spontaneously assembles in vivo into a 3D structure could fight and even help prevent cancer and also infectious disease such as HIV. Their findings are reported in Nature Biotechnology.
“We can create 3D structures using minimally-invasive delivery to enrich and activate a host’s immune cells to target and attack harmful cells in vivo,” said the study’s senior author David Mooney, Ph.D., who is a Wyss Institute Core Faculty member and the Robert P. Pinkas Professor of Bioengineering at Harvard SEAS.
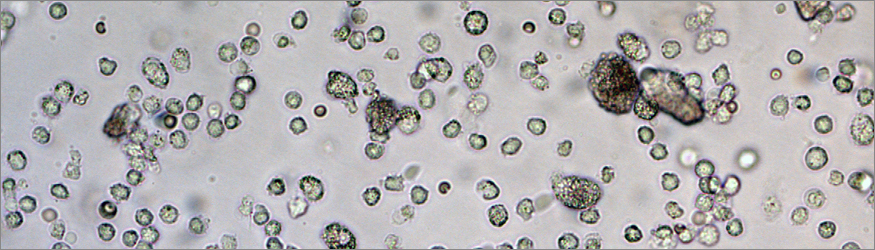
Tiny biodegradable rod-like structures made from silica, known as mesoporous silica rods (MSRs), can be loaded with biological and chemical drug components and then delivered by needle just underneath the skin. The rods spontaneously assemble at the vaccination site to form a three-dimensional scaffold, like pouring a box of matchsticks into a pile on a table. The porous spaces in the stack of MSRs are large enough to recruit and fill up with dendritic cells, which are “surveillance” cells that monitor the body and trigger an immune response when a harmful presence is detected.
“Nano-sized mesoporous silica particles have already been established as useful for manipulating individual cells from the inside, but this is the first time that larger particles, in the micron_sized range, are used to create a 3D in vivo scaffold that can recruit and attract tens of millions of immune cells,” said co-lead author Jaeyun Kim, Ph.D., an Assistant Professor of Chemical Engineering at Sungkyunkwan University and a former Wyss Institute Postdoctoral Fellow.
Synthesized in the lab, the MSRs are built with small holes, known as nanopores, inside. The nanopores can be filled with specific cytokines, oligonucleotides, large protein antigens, or any variety of drugs of interest to allow a vast number of possible combinations to treat a range of infections.
“Although right now we are focusing on developing a cancer vaccine, in the future we could be able to manipulate which type of dendritic cells or other types of immune cells are recruited to the 3D scaffold by using different kinds of cytokines released from the MSRs,” said co-lead author Aileen Li, a graduate student pursuing her Ph.D. in bioengineering at Harvard SEAS. “By tuning the surface properties and pore size of the MSRs, and therefore controlling the introduction and release of various proteins and drugs, we can manipulate the immune system to treat multiple diseases.”
Once the 3D scaffold has recruited dendritic cells from the body, the drugs contained in the MSRs are released, which trips their “surveillance” trigger and initiates an immune response. The activated dendritic cells leave the scaffold and travel to the lymph nodes, where they raise alarm and direct the body’s immune system to attack specific cells, such as cancerous cells. At the site of the injection, the MSRs biodegrade and dissolve naturally within a few months.
So far, the researchers have only tested the 3D vaccine in mice, but have found that it is highly effective. An experiment showed that the injectable 3D scaffold recruited and attracted millions of dendritic cells in a host mouse, before dispersing the cells to the lymph nodes and triggering a powerful immune response.
The vaccines are easily and rapidly manufactured so that they could potentially be widely available very quickly in the face of an emerging infectious disease. “We anticipate 3D vaccines could be broadly useful for many settings, and their injectable nature would also make them easy to administer both inside and outside a clinic,” said Mooney.
Since the vaccine works by triggering an immune response, the method could even be used preventatively by building the body’s immune resistance prior to infection.
“Injectable immunotherapies that use programmable biomaterials as a powerful vehicle to deliver targeted treatment and preventative care could help fight a whole range of deadly infections, including common worldwide killers like HIV and Ebola, as well as cancer,” said Wyss Institute Founding Director Donald Ingber, M.D., Ph.D. who is also Judah Folkman Professor of Vascular Biology at Harvard Medical School and Boston Children’s Hospital, and Professor of Bioengineering at Harvard SEAS. “These injectable 3D vaccines offer a minimally invasive and scalable way to deliver therapies that work by mimicking the body’s own powerful immune-response in diseases that have previously been able to skirt immune detection.”
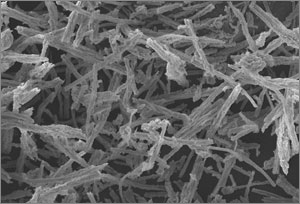
Mesoporous silica rods (MSRs) spontaneously assemble to form a porous 3D scaffold, as seen in this SEM image. The 3D scaffold has many nooks and crannies and is large enough to house tens of millions of recruited immune cells.
Credit: Wyss Institute at Harvard University
Additional co-authors included Youngjin Choi of Sungkyunkwan University in Korea, Sarah A. Lewin of the Wyss Institute, Catia S. Verbeke of Harvard SEAS and the Wyss Institute, and Glenn Dranoff of the Dana-Farber Cancer Institute and Harvard Medical School.
The research was supported by the National Institutes of Health (1R01EB015498), the National Science Foundation, the Wyss Institute for Biologically Inspired Engineering at Harvard University, and the National Research Foundation of Korea.