Bone marrow transplants containing hematopoietic stem cells from an immune-compatible (“allogeneic”) donor can cure patients with otherwise fatal blood disorders including multiple myeloma and leukemias by reconstituting their entire immune systems after chemotherapy. However, following such a “hematopoietic stem cell transplantation” (HSCT), the restoration of T cell immunity – which depends on the production of T cell progenitors in the bone marrow, their migration to the thymus, and differentiation into different T cells lineages – can be delayed by months or sometimes years. This leaves patients vulnerable to infections and other complications. In addition, an immune condition known as graft-versus-host disease (GVHD) can occur when immune cells derived from the donor’s HSCT (graft) attack the patient’s (host) tissues.

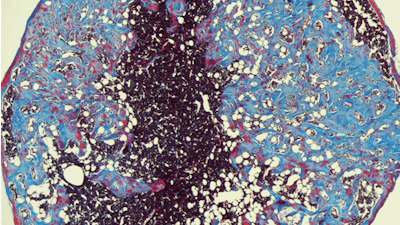
To overcome this problem, a collaborative research team led by David Mooney, Ph.D., at the Wyss Institute and the Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS), and David Scadden, M.D., at Harvard’s Department of Stem Cell and Regenerative Biology has created a material-based approach that can accelerate the full reconstitution of the immune system and adaptive immunity after HSCTs. The approach consists of an implantable “bone marrow cryogel” (BMC), a porous biomaterial-based scaffold that mimics features of normal bone marrow, which is where transplanted stem cells home to after transplantation. Injected under the skin, the BMC releases bone morphogenetic protein 2 (BMP-2), a factor involved in normal bone development, to recruit bone-building mesenchymal cells that help generate a bone-like nodule. Following their transplantation, HSCs home in on the bone-like nodules, multiply in them, and are triggered by a second factor known as Delta-like ligand-4 (DLL4), and displayed by BMCs, to differentiate into progenitor cells for different classes of T cells.

In studies with mice, the team demonstrated that this strategy improved survival and generated T cell progenitors after the animals’ own immune systems had been eradicated and they received HSCTs. The progenitors went on to migrate from the bone-like nodules to the thymus, where they differentiated into functional T cell types, including CD4+ T cells that are commonly limited after HSCTs and vital for adaptive immune responses – for example, against pathogens. Importantly, in addition to having higher numbers and a greater diversity of T cells, the animals could also respond more effectively to an immune-challenging model vaccine (antigen) and showed weaker signs of GVHD triggered by HSCTs than animals that had received control cryogels loaded with neither of the two factors or only BMP-2. The BMC approach could provide an off-the-shelf solution for enhancing T cell regeneration and mitigating GVHD in HSCT in patients with severe blood disorders.